Medicaid waiver programs vary by state, each focusing on unique strategies to improve access and quality. For example, Alabama emphasizes community outreach and provider partnerships, while California uses innovative technology and personalized care models. Texas highlights telehealth and growth mindset, and New York expands home care and behavioral health options. Funding and policies influence what’s available, so exploring each state’s approach can help you understand how they serve their residents. To find out more, keep exploring these detailed state differences.
Key Takeaways
- Medicaid waiver programs vary by state, focusing on community-based, patient-centered, and integrated care models.
- States leverage innovative strategies like telehealth, AI tools, and digital platforms to enhance service delivery.
- Eligibility requirements typically include income, disability status, and residency, with specific application processes per state.
- State policies and funding allocations significantly influence program scope, expansion efforts, and target populations.
- Common focus areas include behavioral health, long-term care, community outreach, and reducing hospitalizations through tailored initiatives.
Alabama Medicaid Waivers

Alabama Medicaid Waivers allow eligible residents to access specialized services beyond standard Medicaid coverage. To make these services available, the program emphasizes community outreach, guaranteeing residents are aware of available options. Outreach efforts include local events, informational campaigns, and direct engagement with community organizations. These initiatives help connect individuals to the appropriate resources and support. Provider partnerships also play an essential role, as Alabama collaborates with healthcare providers, social service agencies, and community organizations to deliver comprehensive care. By fostering strong relationships with trusted providers, the state guarantees that participants receive personalized, effective support tailored to their needs. Additionally, hours of operation are coordinated to ensure timely access to services. Together, community outreach and provider partnerships help Alabama Medicaid Waivers extend critical services to those who need them most.
California’s Innovative Approaches

California has pioneered innovative strategies to expand access to Medicaid services, leveraging technology and personalized outreach to reach underserved populations. The state emphasizes innovative care models that focus on community-based, patient-centered solutions. Technology integration plays a vital role, enabling streamlined communication, telehealth services, and data collection to improve overall care coordination. California’s approach emphasizes proactive engagement, using digital platforms to connect vulnerable populations with resources and support. These efforts help reduce barriers to care, especially for rural and low-income communities. By adopting innovative care models and integrating technology, California aims to make Medicaid services more accessible, efficient, and responsive to individual needs. This forward-thinking approach sets a benchmark for expanding Medicaid access through creative, tech-driven solutions. Additionally, the use of airless paint sprayers as a metaphor highlights the importance of adopting advanced and efficient tools to improve service delivery and outreach effectiveness.
Texas Medicaid Demonstrations

How are Texas Medicaid demonstrations shaping innovative ways to expand access and improve services? These programs leverage telehealth innovations to reach underserved populations, making healthcare more accessible, especially in rural areas. By fostering strong provider partnerships, Texas ensures that services are coordinated and patient-centered. The demonstrations encourage providers to adopt new technologies and delivery models, reducing barriers like transportation and wait times. As a result, beneficiaries experience more convenient, timely care, which can lead to better health outcomes. Additionally, these initiatives help control costs while maintaining quality. Incorporating growth mindset principles, Texas’s approach demonstrates how combining telehealth innovations with strategic provider partnerships can transform Medicaid services, making healthcare more equitable and efficient for those who need it most.
New York State Programs
New York State’s Medicaid waiver programs are pioneering innovative strategies to expand access and enhance the quality of care. These programs emphasize improving home care options, allowing more individuals to receive services in their own homes rather than institutions. They also focus heavily on behavioral health, addressing mental health needs alongside physical health. Through targeted initiatives, you can access extensive support that integrates behavioral health services with primary care, reducing hospitalizations and promoting recovery. The state’s approach encourages community-based solutions, empowering you to receive personalized care tailored to your needs. By expanding home care and behavioral health options, New York aims to create a more inclusive, effective Medicaid system that supports your well-being and independence. Additionally, these programs often incorporate all water parks, offering innovative recreational and therapeutic activities to enhance quality of life.
Florida’s Medicaid Expansion Efforts
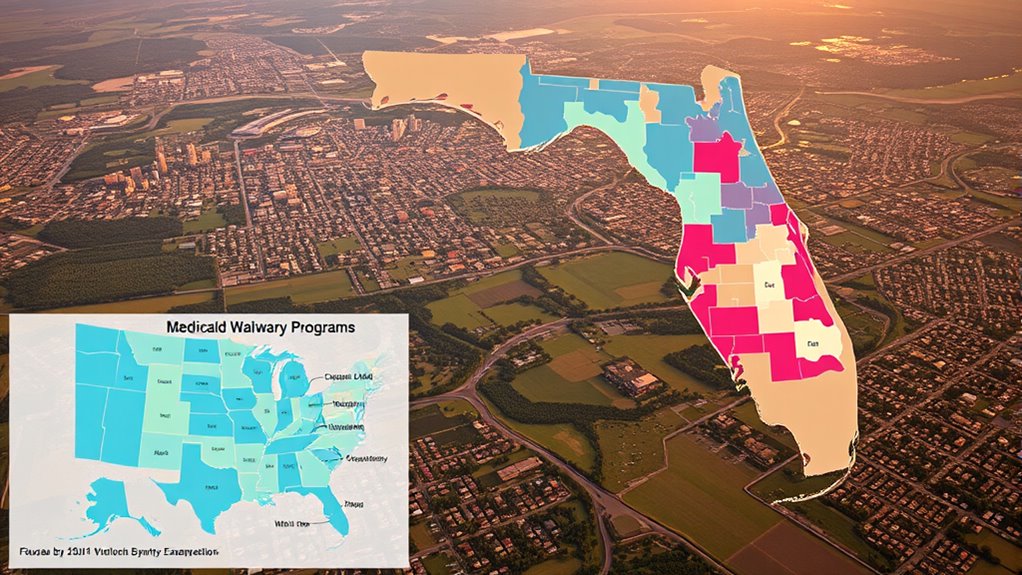
Florida is working to expand its Medicaid program, but the eligibility criteria and funding sources are key factors to watch. Policy changes are shaping how many residents can benefit and how the program is financed. Understanding these points helps you see how the expansion might impact access to healthcare in the state. Supporting elderly independence is an important aspect of these initiatives, aiming to improve quality of life for aging residents.
Expansion Eligibility Criteria
Are you wondering who qualifies for Medicaid under Florida’s waiver programs? Eligibility primarily depends on income thresholds and demographic restrictions. If your income falls within the specified limits—often up to 138% of the federal poverty level—you may qualify. Florida’s waiver programs target specific populations, such as low-income adults, pregnant women, or individuals with disabilities, based on demographic restrictions. These criteria can vary depending on the program’s goals and funding. Some waivers prioritize certain age groups or health conditions, while others focus on geographic areas. It’s essential to review the specific eligibility requirements for each waiver, as they determine who can access expanded Medicaid benefits under Florida’s efforts. Additionally, understanding the residency requirements in each state, such as the 6-month residency in Florida, is crucial for qualifying.
Funding and Policy Changes
Recent policy shifts and funding adjustments have considerably impacted Medicaid expansion efforts in Florida. Legislative changes and budget adjustments influence how funds are allocated, shaping the scope of expansion. These shifts can either accelerate or hinder progress, depending on political priorities and economic conditions. For example, recent legislative decisions may:
- Limit funding for certain programs
- Reallocate resources to other health initiatives
- Introduce new eligibility criteria
- Adjust provider reimbursement rates
- Delay expansion deadlines
Understanding these changes helps you grasp the evolving landscape of Florida’s Medicaid efforts. Ongoing budget adjustments reflect the state’s commitment to balancing fiscal responsibility with healthcare access. Staying informed about legislative developments ensures you’re aware of potential opportunities or barriers in Medicaid expansion. Additionally, the contrast between static and dynamic contrast ratio considerations can influence how effectively the program addresses diverse healthcare needs.
Illinois Custom Coverage Initiatives

Illinois offers a variety of Medicaid program options tailored to different needs. You’ll find specific eligibility requirements and an straightforward enrollment process to access these services. Understanding these initiatives helps you make informed decisions about your healthcare coverage. Being aware of grocery store hours can also assist in planning your shopping trips efficiently around your healthcare appointments.
Illinois Program Offerings
Curious about how Illinois tailors its Medicaid services? The state offers a variety of custom coverage initiatives designed to meet diverse needs. These programs focus on:
- Enhancing community outreach efforts to connect underserved populations
- Building strong provider partnerships for better care coordination
- Offering specialized services for chronic conditions
- Supporting behavioral health and mental health programs
- Facilitating home and community-based services
- Incorporating innovative AI-enabled solutions to improve service delivery and efficiency.
Illinois emphasizes collaboration with local organizations and healthcare providers to improve access and quality. Through these tailored initiatives, you can benefit from expanded services that address unique community needs. The state’s proactive approach helps ensure that Medicaid recipients receive thorough, personalized care, making healthcare more accessible and effective for everyone involved.
Eligibility Requirements
How do you determine if you qualify for Illinois’s tailored Medicaid coverage initiatives? First, your income verification must fall below certain thresholds, ensuring your income aligns with program limits. Additionally, meeting disability criteria is essential if the initiative targets individuals with disabilities; you’ll need documented proof of disability that qualifies under program standards. These initiatives often have specific eligibility rules, so it’s important to review the criteria carefully. Income verification involves providing recent financial documentation, while disability assessments require medical records or evaluations. If you meet both the income and disability requirements, you may be eligible for customized coverage options designed to address your unique health needs. Regularly reviewing application requirements can help ensure you meet all necessary criteria before applying. Always check with Illinois’s Medicaid office to confirm your eligibility based on these criteria.
Enrollment Process
Ready to enroll in Illinois’s tailored Medicaid coverage initiatives? The enrollment process is straightforward if you understand the steps involved. First, you’ll need to complete the application procedures, which include submitting your personal information and supporting documents. The state will verify your eligibility through an eligibility verification process to confirm you meet the criteria. To make it easier, consider these points:
- Gather necessary documentation beforehand
- Complete online or in-person applications
- Respond promptly to any follow-up requests
- Use the Illinois Medicaid portal for updates
- Contact local offices for assistance
Understanding these steps ensures a smooth enrollment experience. Remember, accurate eligibility verification is key to qualifying for Illinois’s custom coverage initiatives, so double-check your information and stay proactive throughout the process.
Ohio’s Managed Care Waivers

Have you ever wondered how Ohio manages its Medicaid services to better meet the needs of its residents? Ohio’s managed care waivers focus on improving access to essential services like long-term care and behavioral health support. These waivers allow the state to coordinate care more effectively, ensuring individuals receive personalized attention. They also help control costs while maintaining quality.
| Personal Impact | Ohio’s Managed Care Waivers |
|---|---|
| Better access | More support for long-term care needs |
| Improved care | Enhanced behavioral health services |
| Cost savings | Efficient resource management |
| Individualized | Tailored plans for diverse needs |
| Community support | Strengthening local healthcare systems |
Pennsylvania’s Access Enhancements

Pennsylvania has made significant improvements to its Medicaid access through targeted enhancements designed to reduce barriers and expand support. These efforts focus on strengthening provider partnerships and advancing service integration, making care more seamless. By collaborating closely with healthcare providers, the state guarantees better coordination of services and reduces gaps in care. Service integration allows beneficiaries to access multiple supports within a single, cohesive system, improving overall health outcomes. Key features include expanded provider networks, streamlined enrollment processes, telehealth options, culturally competent services, and enhanced care management. These enhancements make it easier for individuals to connect with the right providers, receive comprehensive support, and navigate the complex healthcare landscape more effectively. The result is a more accessible, integrated Medicaid system tailored to meet diverse needs.
Washington State’s Targeted Services

Washington State has focused on developing targeted services to address specific health and social needs of its Medicaid populations. These efforts primarily aim to improve behavioral health outcomes and support community integration. By tailoring programs to meet unique needs, you can access specialized behavioral health services that promote recovery and stability. The state emphasizes community-based approaches, helping you stay connected and engaged within your local environment. These targeted services include outreach, crisis intervention, and peer support, all designed to reduce hospitalization rates and improve quality of life. Through these initiatives, you’re encouraged to participate actively in your community, fostering independence and social inclusion. Overall, Washington’s targeted services aim to provide exhaustive, accessible care that empowers you to achieve better health and stronger community ties.
Frequently Asked Questions
How Do States Evaluate the Success of Their Medicaid Waiver Programs?
You evaluate your Medicaid waiver program’s success by analyzing quality metrics like health outcomes and service delivery efficiency. You also gather stakeholder feedback from participants, providers, and families to understand their experiences. Combining these insights helps you identify areas for improvement and measure progress over time. This ongoing assessment guarantees your program effectively meets community needs while maintaining high standards of care and operational performance.
What Are the Eligibility Criteria for Participating in Medicaid Waivers?
Think of eligibility criteria like a gatekeeper, deciding who can enter the program. You typically need to meet income requirements, which vary by state, and disability criteria that qualify you for specific waivers. If your income is low enough and you have a qualifying disability, you’re likely to be eligible. These criteria guarantee that those who need help the most can access Medicaid waivers to get essential support.
How Do Waiver Programs Impact Overall Medicaid Spending and Budgets?
You’ll find that waiver programs impact overall Medicaid spending by offering budget flexibility, allowing states to allocate funds more efficiently. This flexibility promotes program innovation, enabling tailored services that meet specific needs without overspending. While they can increase short-term costs, they often lead to long-term savings by preventing costly institutional care. Overall, waiver programs balance budget considerations with innovative approaches, improving care quality and controlling Medicaid expenditures effectively.
Can Beneficiaries Access Multiple Waiver Programs Simultaneously?
Ever wonder if you can access multiple waiver programs at once? It depends on the state’s rules, as program overlap and waiver coordination vary. Some states allow beneficiaries to participate in several programs simultaneously to maximize benefits, while others restrict this to prevent duplication. You should check with your state’s Medicaid office to see what’s possible in your area, since policies differ and may change over time.
What Are Common Challenges States Face When Implementing Medicaid Waivers?
When implementing Medicaid waivers, you might face common challenges like funding constraints that limit program expansion or sustainability. Additionally, engaging stakeholders—such as providers, beneficiaries, and policymakers—can be difficult but is essential for success. These obstacles require careful planning and communication to navigate effectively. By addressing funding issues early and fostering stakeholder engagement, you can improve the chances of successful waiver implementation and better serve your community’s needs.
Conclusion
As you explore these state Medicaid waivers, it’s almost amusing to see how each claims to innovate and improve care. In reality, many programs resemble a game of political chess, with policies shifting like pieces on a board. You might picture a patchwork quilt of efforts—some colorful, some frayed—intended to cover everyone, yet often leaving many still exposed. Ironically, in chasing better access, some programs seem more about appearances than real change.